This article explains how periodontal disease can develop and the different stages. We discuss who to see for periodontal disease treatment and what to expect.
What Is Periodontal Disease?
Gum or periodontal disease is a bacterial infection that destroys gum tissue and the bone around your teeth. It can be caused by lax oral care.
The aim of twice daily brushing and flossing your teeth once a day is to remove the buildup of dental plaque, a sticky biofilm containing harmful and infectious bacteria. Plaque is continually forming over your teeth.
If you don’t brush and floss regularly and thoroughly, plaque will continue to build up. It hardens into tartar or calculus within a couple of days. Plaque and tartar contain the bacteria that cause periodontal disease.
Read more: The Pros and Cons of a Dental Bridge
How Does Periodontal Disease Develop?
The bacteria in plaque and tartar feast on leftover food particles trapped on and around your teeth, creating toxins as they thrive. These bacteria will infect and inflame your gums, gradually destroying them.
As more tartar buildup, it makes it easier for plaque to adhere to your teeth. Plaque and tartar tend to accumulate around the gumline, where your teeth meet your gums. When the disease worsens, it can destroy your gums and structures supporting your teeth, including your jawbone.
Periodontal disease is a major cause of tooth loss. It’s also extremely common, and around half of all adults will develop some form of gum disease during their lifetime.
Read more: Why Does It Pain Two Weeks After Your Dental Bone Graft
Symptoms of Periodontal Disease
When your gums are healthy, they should be pink and fit snugly around your teeth. They should never look swollen, and healthy gums should never bleed.
Initially, periodontal disease can cause few symptoms, so it is often called a silent disease.
However, as it progresses, symptoms can include:
- Red or purple gums.
- Bleeding when brushing or flossing or at other times.
- Gums that feel tender to touch.
- Swollen gums.
- Bad breath.
- An unpleasant taste.
- Pain or discomfort when chewing.
- Teeth that look longer as gums recede.
- Changes to the way your teeth bite together.
- Loose teeth.
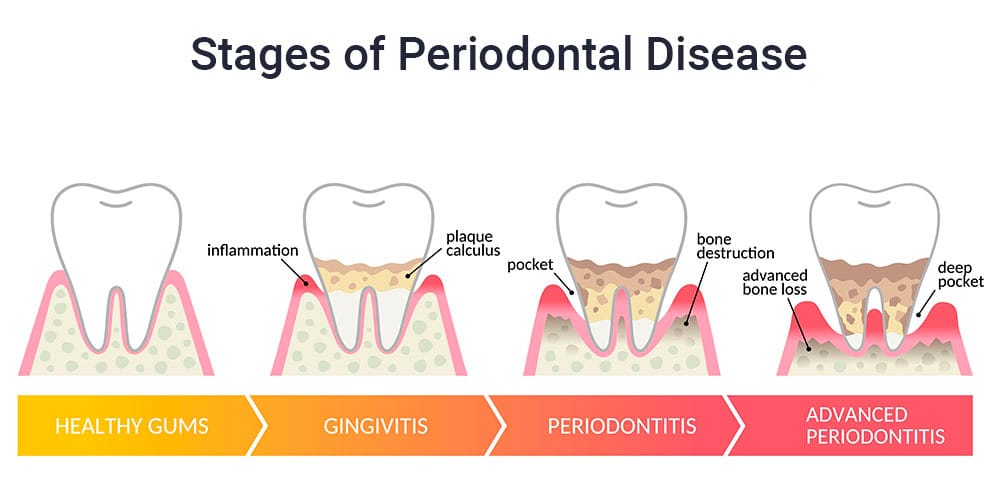
There are four distinct stages of periodontal disease.
Understanding the Different Stages of Periodontal Disease
The four different stages are outlined below.
Mild Gum Disease or Gingivitis
Gingivitis is the very first stage of gum disease. You might notice your gums look a bit swollen or puffy. They could start to look red and might bleed during brushing and flossing.
Ideally, you will notice these symptoms and seek professional dental care before permanent damage to your gums and jawbone can occur.
At this point gingivitis is reversible with proper professional care and improved oral care at home. More advanced gum disease can cause irreversible damage and may be chronic.
Read more: What Happens During a Dental Crown Procedure?
Mild Periodontitis
When gingivitis progresses, it develops into mild periodontitis, where the bacteria penetrate your gums. At this point, they can begin to impact your jawbone.
Gum recession occurs as the inflammation caused by bacteria destroys your gums. You may notice your gums start pulling away from your teeth as they recede, creating periodontal pockets.
These pockets can harbor harmful bacteria as they provide the ideal environment for them to thrive. Also, they can be quite deep and cannot be cleaned by your toothbrush or dental floss.
Moderate Periodontitis
Unless you seek treatment, the bacteria will continue to destroy your gum and jawbone as the disease progresses. The bacteria will also start to destroy the periodontal ligaments, which are stretchy pieces of tissue that hold your teeth in their sockets.
By this stage, you may notice you have permanent bad breath. Your teeth and gums may begin to feel painful and tender. Pus can develop around the gumline.
Advanced Periodontitis
As the infection and inflammation worsen, the destruction of your jawbone and gums continues. Eventually, your teeth will become loose and may even fall out.
It’s also worth mentioning the potential impact on your general health. As your gums bleed, harmful bacteria can enter your bloodstream and travel around your body.
Once in your blood, these bacteria can create new sites of inflammation and infection. They can increase your risk of developing serious health problems, including heart disease and diabetes. If you have any existing health problems, these could worsen.
Diabetes is a good example; if poorly controlled, it can increase the glucose in your saliva, feeding the bacteria that cause periodontal disease. If you have periodontal disease, it can make it harder to control diabetes, setting up a vicious cycle that impacts your overall and oral health.
Who Can Develop Periodontal Disease?
most cases of periodontal disease are caused by poor oral care, some people are more at risk than others.
Risk factors can include:
- Smoking.
- Conditions that suppress the immune system make fighting infections like periodontal disease harder.
- Heart disease.
- Diabetes.
- Hormonal changes as these increase the sensitivity of gum tissue to plaque bacteria.
- Stress.
- Genetics, so if your parents or siblings have this disease, your risk can be higher.
How Is Periodontal Disease Diagnosed?
Your general or family dentist can diagnose periodontal disease during a routine dental checkup. They can identify the symptoms during your dental exam and assess the degree of infection and inflammation.
The dentist will use a periodontal probe to measure the size and depth of pockets around your teeth. These measurements enable them to assess the extent of the damage to your gum and bone. The deeper the pockets, the greater the severity of the infection.
You will almost certainly need dental X-rays. These are useful in showing where jawbone loss has already occurred and can be compared with previous X-rays to show how your jawbone has changed.
How Is Periodontal Disease Treated?
The treatment recommended will depend on the degree of infection. If you have gingivitis, treatment is straightforward and inexpensive.
Gingivitis Treatment
Treating gingivitis will involve a professional dental cleaning and improved oral hygiene at home. Your hygienist may wish to review your oral care routine with you and can offer useful advice on improving it.
It’s important to persevere afterward by brushing your teeth at least twice daily and flossing daily. You may find that initially, your gums bleed slightly, but if you continue, they will get healthier and stronger within a few weeks, and the bleeding will cease.
While a general dentist can successfully treat gingivitis, you may require more specialized care for mild, moderate, or advanced periodontal disease.
Seeing a Periodontist for Treatment
Your dentist may refer you to a periodontist, a dental specialist who treats conditions affecting structures around your teeth, including periodontal disease. Alternatively, you may visit a periodontist directly, as you do not need a referral.
The advantage of seeing a periodontist is receiving the most up-to-date and advanced periodontal care, which can be especially important if you have severe gum disease. A periodontist has years of advanced training, and their dental office will be equipped with the latest technologies to ensure you get the very best periodontal treatment.
Read more: The 8 Best Alternatives to Invisalign
Treating Periodontal Disease
Several treatments are available for periodontal disease, which are outlined below.
Scaling and Root Planing
Treatment is similar to an ordinary hygiene appointment but is designed to deeply clean your teeth and gums.
Instead of just cleaning your teeth by scaling them, the process cleans any exposed tooth roots by scaling them carefully before these surfaces are smoothed or planed. Smoothing these surfaces makes it easier for gums to reattach and harder for bacteria to stick to teeth and tooth roots.
Sometimes, treatment is completed in a single visit, but if the infection is severe, your periodontist may suggest several visits and use a local anesthetic to ensure you feel comfortable.
Osseous Surgery
Also called pocket reduction surgery, this treatment may be necessary if you have more moderate or advanced periodontal disease.
Treatment is designed to remove plaque and tartar from deep underneath your gums by creating a flap in your gum tissue. The flap is then moved back from your tooth roots, allowing them to be thoroughly cleaned and smoothed.
Once cleaned, your gum tissue is repositioned and stitched shut. This procedure is often used with other treatments like laser dentistry or procedures designed to help tissue regenerate, such as bone and gum grafting.
LANAP
Laser-Assisted New Attachment Procedure (LANAP) is an advanced dental laser treatment. The laser helps sterilize gums while removing unhealthy tissues, leaving healthy tissue intact. Afterward, as infection is reduced, your gums will begin to fit more snugly around your teeth.
Bone Grafts
If advanced gum disease has destroyed your jawbone, a bone graft can help replace it. The bone graft acts as a matrix or scaffold, encouraging your body to produce new bone cells that gradually replace it.
Gum Grafts
Gum graft surgery uses tissue to cover exposed tooth roots, helping to improve gum health and create a more aesthetically pleasing appearance. The grafting tissue can be taken from the roof of your mouth, or some periodontists may use a tissue bank. The tissues supplied by a tissue bank are extensively sterilized and treated to be safe for use.
Ongoing Treatment for Chronic Periodontitis
It isn’t always possible to cure periodontal disease entirely. Therefore, your periodontist may provide you with an ongoing dental care plan, and you might need to visit them regularly for scaling and root planing or other maintenance treatments.
Periodontitis Is Preventable
Ideally, it’s better to prevent this condition, and you can do that by making sure you see your dentist regularly for dental exams and hygiene appointments. Regular dental checkups ensure any early signs of gum disease are detected quickly and treated promptly.
However, if you are concerned about your gum health, consider seeing a periodontist for a proper evaluation.

